Breakthroughs in Immunotherapy in cancer treatment
Immunotherapy has revolutionized cancer treatment by leveraging the body’s own immune system to identify and destroy cancer cells. Unlike traditional therapies like chemotherapy and radiation, which directly target cancer, immunotherapy empowers the immune system to recognize and combat malignancies. Recent advancements in cancer treatment have significantly improved patient outcomes and quality of life.
Checkpoint inhibitors have emerged as a pivotal advancement in immunotherapy. These drugs, such as pembrolizumab and nivolumab, work by blocking proteins that prevent T-cells from attacking cancer cells. By inhibiting these checkpoints, T-cells can more effectively target and eliminate cancerous cells. Clinical trials have shown remarkable success in treating melanoma, non-small cell lung cancer, and renal cell carcinoma with checkpoint inhibitors.
CAR T-cell therapy represents another significant breakthrough. This personalized cancer treatment involves extracting a patient’s T-cells, genetically modifying them to express chimeric antigen receptors (CARs), and then reinfusing them into the patient. These engineered T-cells can specifically target and destroy cancer cells. CAR T-cell therapy has shown substantial efficacy in treating certain blood cancers, such as acute lymphoblastic leukemia and non-Hodgkin lymphoma.
Cancer vaccines are also making strides, aiming to prompt the immune system to recognize and attack cancer cells. Unlike traditional vaccines that prevent diseases, cancer vaccines are therapeutic, designed to treat existing cancer. Sipuleucel-T is a notable example, approved for prostate cancer treatment. Recent studies have also explored vaccines for ovarian and breast cancers, showing promising results for cancer treatment.

Recent clinical trials spotlight the efficacy and safety of these immunotherapies. For instance, a study published in the New England Journal of Medicine demonstrated that combining checkpoint inhibitors with chemotherapy significantly improved survival rates in patients with advanced lung cancer. Another trial highlighted the long-term remission achieved with CAR T-cell therapy in patients with refractory lymphoma.
While the progress in immunotherapy is encouraging, it is not without challenges. Side effects, such as immune-related adverse events, can be severe and require careful management. Additionally, not all cancer types respond equally to immunotherapy, necessitating ongoing research to broaden its applicability.
Future directions in immunotherapy research aim to enhance its effectiveness and accessibility. Efforts are focused on identifying biomarkers that predict patient response, developing combination therapies to overcome resistance, and reducing treatment costs. As research advances, immunotherapy holds the promise of transforming cancer care for a wider range of patients, offering hope for improved outcomes and quality of life.
Innovations in Targeted Therapy
Targeted therapy represents a significant advancement in cancer treatment, diverging fundamentally from traditional chemotherapy. Unlike chemotherapy, which indiscriminately attacks rapidly dividing cells, targeted therapy employs drugs designed to pinpoint and disrupt specific genes or proteins that contribute to cancer cell proliferation and survival. This precision not only enhances treatment efficacy but also minimizes collateral damage to healthy cells.
One of the most notable breakthroughs in targeted therapy in cancer treatment is the development of tyrosine kinase inhibitors (TKIs). These drugs obstruct the function of tyrosine kinases, enzymes that play a crucial role in signal transduction pathways, thereby curbing cancer cell growth. Imatinib (Gleevec), a TKI designed for chronic myeloid leukemia (CML), has transformed CML from a fatal disease into a manageable condition for many patients. Clinical trials have shown significant improvement in survival rates, underscoring the potential of TKIs.
ALSO READ THIS : Wholesome Eats: Nourish Your Body with Superfoods and Immune-Boosting Recipes
Monoclonal antibodies represent another milestone in targeted therapy. These laboratory-made molecules can bind to specific targets on cancer cells, marking them for destruction by the immune system. Trastuzumab (Herceptin), used in treating HER2-positive breast cancer, has demonstrated remarkable success, with numerous clinical trials reporting improved patient outcomes and prolonged survival rates.
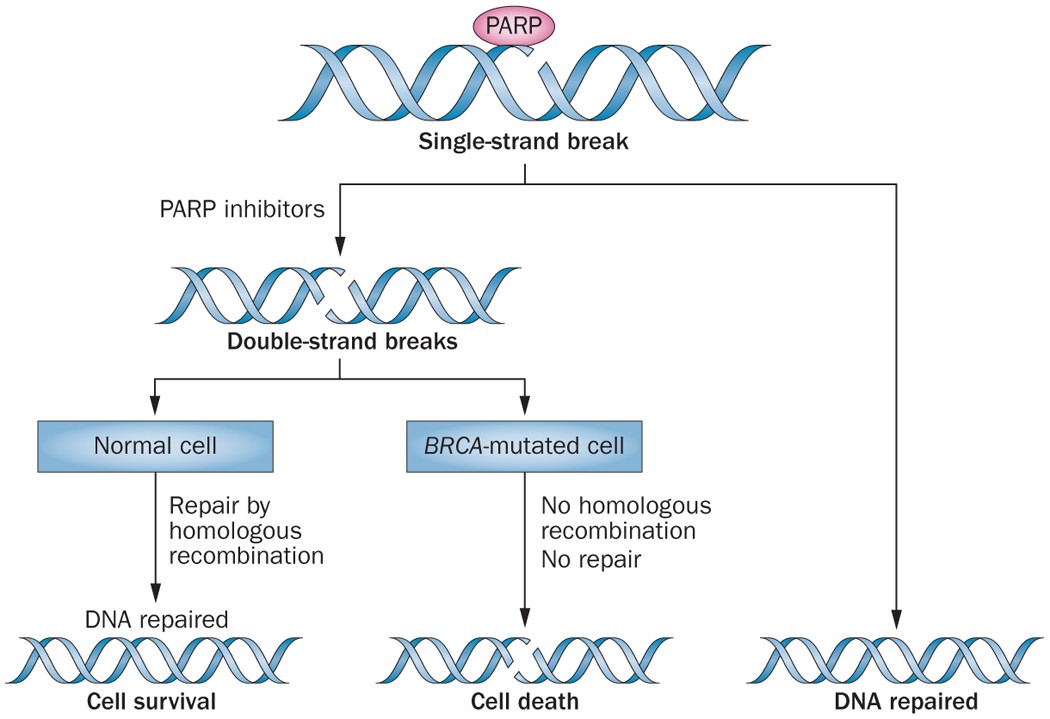
PARP inhibitors, another class of targeted therapies, have shown efficacy particularly in cancers with BRCA1 or BRCA2 mutations. These inhibitors impair the cancer cells’ ability to repair DNA damage, leading to cell death. Olaparib (Lynparza) is a PARP inhibitor that has been effective in treating ovarian and breast cancers, offering a promising option for patients with these specific genetic profiles.
Despite these advancements, the development of targeted therapies is not without challenges. Drug resistance remains a significant hurdle, as cancer cells can mutate and develop resistance to treatment. Additionally, ensuring the specificity of these treatments to avoid off-target effects is a complex task. Researchers are continually working to overcome these obstacles, focusing on refining drug design and exploring combination therapies to enhance effectiveness.
Ongoing research in targeted therapy is pushing the boundaries of personalized medicine. By integrating genomic data and patient-specific factors, future therapies aim to offer more tailored and effective treatments. Innovations such as CRISPR gene editing and next-generation sequencing hold promise for the next wave of breakthroughs, potentially revolutionizing cancer treatment and improving patient outcomes even further.